Body Balance Quarterly (The BBQ)
The Opioid Crisis Leads Canadians to Seek Alternative Approaches for the Management of Chronic Pain
The Opioid Crisis
In December 2017, a Canadian news report released by CBC news made citizens aware of the rising number of opioid related deaths over the past year. Rising from 2,861 opioid related fatalities in 2016, based on the information reported to the Public Health Agency of Canada, it was projected that Canada was on track to see over 4000 deaths from opioid toxicity at the closing of 2017 (The Canadian Press, 2017). With the rising number of opioid fatalities each calendar year this has caused significant controversy among the Canadian Government, health care professionals, and citizens over the prescription of opioids and the use of these substances in the management of chronic pain.
In light of the unfolding opioid crisis, and the unveiling of the topic of ‘Chronic Pain’ among the recent news headlines in this edition of the Body Balance Quarterly we would like to offer our perspective on chronic pain. We will also discuss the latest evidence in support of alternative methods for chronic pain management.
What is Chronic Pain?
Pain is a complex phenomenon that extends far beyond a standardized feeling of discomfort and soreness. Pain is a subjective and emotional experience, which is characterized differently in every individual. In cases of Acute Pain that is felt following an injury, a signal of tissue damage is sent to the brain. In acute pain cases, the pain felt is typically proportional to the amount of tissue that has been damaged. When people experience pain after an injury, pain is believed to be a useful stage of the healing process as it promotes rest, which ultimately promotes healing. However, in cases of chronic pain the link between the presence of tissue damage and one’s pain levels becomes disconnected.
Until recently, the topic of ‘Chronic Pain’ has not been a hot topic of conversation among the general population. However, even with its increased prevalence in the news today with the current opioid crisis, the concept of chronic pain is still an idea that is not well understood by many. Chronic pain conditions include fibromyalgia, chronic regional pain syndrome (CRPS), spinal pain, and chronic low back pain (among many others). In cases of chronic pain, the pain experienced by an individual extends beyond the typical healing time of newly damaged tissue. In individuals with chronic pain the nervous system becomes hypersensitive to incoming signals causing the pain system to be ‘Turned up’, which reduces an individual’s pain threshold. This ultimately causes an individual to experience pain with tasks or sensations that would not normally be perceived as painful. This can have significant impacts on daily life as it causes increased attention to painful regions, reduced activity levels and subsequently activity tolerance, heightened stress response, poor concentration as well as sleep disturbances. Without intervention this can lead to a cumulative and chronic pain cycle leading to overall deconditioning which further amplifies the effects of chronic pain conditions (WRIISC, 2014).
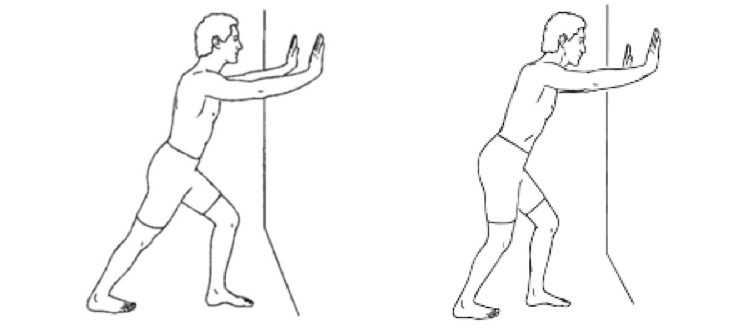
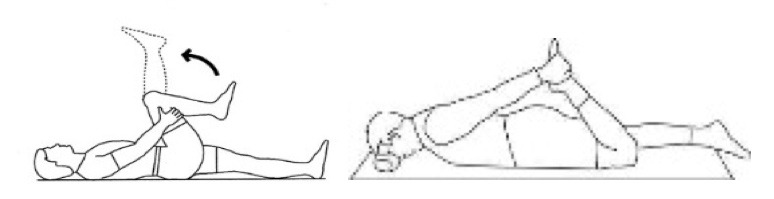
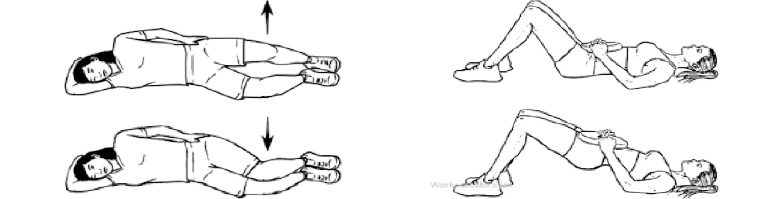
So what can be done to break this pain cycle? Over the course of the past 5 years, an increased volume of literature has been devoted to the benefits of low – moderate intensity exercise, in the management of chronic pain symptoms. In a recent literature review Geenen et al. (2017) concluded that a general exercise and strengthening program has proven to be effective among individuals with chronic pain conditions in improving both pain severity and overall quality of life. However, self-initiated exercise programs were found to be less effective among this same population (Geenen et al. 2017). Numerous exercise interventions were included among this review from aerobic exercise, strength training and flexibility, to range of motion exercises, balance training, core strengthening, tai chi, yoga and pilates, which displays the wide variety of successful exercise options available (Geenen et al. 2017).
Mechanism of How Exercise Aids in Managing Chronic Pain Symptoms
‘Exercise is medicine’ has been a popular phrase among health care professionals and health advocates among recent years. In cases of chronic pain, exercise has proven to display many benefits in helping to manage chronic pain symptoms. Above we talked about how individuals living with chronic pain have a hypersensitive nervous system causing the pain system to be ‘Turned up’. The goal of exercise is to help retrain the pain system to be ‘Turned down’ by calming the nervous system and reducing its sensitivity to incoming signals. The human body is designed to move, and by introducing graded exercise and daily pacing strategies this can play a substantial role in the management of you or your loved one’s chronic pain symptoms.
Exercise helps to increase your energy stores, giving you a longer charge or battery life. This will help reduce your fatigue levels and make it easier for you to perform your daily activities. Aside from the benefits of pain reduction alone, there are numerous other health benefits that exercise has to offer, including but not limited to; decreased blood pressure and resting heart rate—ultimately lowering one’s risk of developing heart disease or stroke—improved sleep, weight loss, increased muscle mass, as well as improved psychological well being.
Among individuals living with chronic pain conditions, a common misconception is that exercise attempts will cause a flare up of pain symptoms, and therefore these individuals often rely on rest and relaxation to avoid worsening of pain symptoms (WRIISC, 2014). However, for successful long-term management of chronic pain conditions, a low to moderate intensity exercise program should be introduced. Here are some tips to consider with regards to exercising if you or a loved one has been experiencing chronic pain. Remember, although opioids may not be the answer for managing chronic pain, today’s evidence supports that exercise is!
Tips On Exercising Safely and Effectively for Chronic Pain Management
1) Contact your doctor first to determine whether or not you are ready for exercise and to begin exercising safely. It is very important to exercise with proper form and technique in order to prevent injury and training the wrong muscle patterns. If you are unsure about how to exercise safely follow up with a health care professional to get you started on a safe and individualized exercise routine.
2) Gradual exposure to exercise is very important to not ‘flare up’ the pain system. It is important to remember that in the beginning stage of exercise you may experience some worsened symptoms during or after exercising, however, if the pain is too severe that you feel you cause a ‘flare up’ you have likely done too much (Geenen et al. 2017). If you feel abnormally fatigued or have pain symptoms that are more significant than usual, take a break from exercising and return to exercise when your symptoms have decreased.
3) The effects of exercise often may take longer to display in individuals who are dealing with chronic pain (Geenen et al. 2017). Remember to be patient, by choosing a form of exercise you enjoy it will make exercise seem less daunting.
4) Gradually increase the exercise volume before you increase the overall exercise intensity. Once you are able to exercise daily, then slowly increase the difficulty of your exercise routine.
5) Include exercises that target all areas of the body, and all large muscle groups.
If you have a chronic pain condition and are ready to begin an exercise routine but are not sure where to start we can help! Body Balance Health offers numerous Health and Wellness programs to help develop an individualized exercise program for you to begin exercising safely. Check out our website or give us a call to see if Body Balance Health’s programs are right for you!
Body Balance Health & Physiotherapy News
In other Body Balance Health & Physiotherapy News, we would like to welcome Conor O’Flynn to the Body Balance team! Conor is a manual osteopath who will be joining the clinic twice weekly (Tuesday’s & Thursday’s). Conor’s therapeutic work focuses on musculoskeletal issues of all kinds. Conor also has experience working with individuals who have been experiencing chronic pain. Osteopathy uses manual (hands on) therapeutic techniques to restore balance and integrity to the body by removing the barriers to healing and recovery.
Works Cited
Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database of Systematic Reviews 2017, Issue 4. Art. No.: CD011279. DOI: 10.1002/14651858.CD011279.pub3
The Canadian Press. (December 18, 2017). Opioid deaths in Canada expected to hit 4,000 by end of 2017. CBC News. http://www.cbc.ca/news/health/opioid-deaths-canada-4000-projected-2017-1.4455518
The Government of Canada. (August 29, 2017). Apparent Opioid-Related Deaths in Canada in 2016*. Public Health Agency of Canada. https://www.canada.ca/content/dam/hc-sc/documents/services/publications/healthy-living/opioids-infographic-eng.pdf
War Related Illness & Injury Study Centre. (March, 2014). Exercise to help manage chronic pain and/or fatigue. Veterans Health Administration: Office of Public Health. https://www.warrelatedillness.va.gov/education/factsheets/exercise-to-manage-pain.pdf